The core principle of user-centricity embraced by designers resonates with the HSE Digital Health Strategic Implementation Plan (1) and HSE Digital Roadmap (2), (among other reports), which aim to improve health experiences and accessibility of digital health in Ireland. By delving into the ‘how’ and ‘why’ of user needs, while also considering broader societal requirements and long-term strategies and policies, designers will play a pivotal role in supporting the pursuit of improved access, inclusion, consistency, and utilisation of healthcare in 2024. In the context of Ireland’s ongoing digital health transformation, embracing user-centred design principles can drive innovation, efficiency, and effectiveness in healthcare. By prioritising the needs and perspectives of patients and healthcare providers through design, a more inclusive and user-centric healthcare system that truly puts the individual at the heart of innovation can be achievable.
This article explores the shape of health in Ireland, and how design has a role to play in the digital transformation of health services – in relation to better access and inclusion.
Health in Ireland
Ireland has one of the highest rates of avoidable admissions for asthma and COPD, high addiction rates, high levels of antibiotic prescribing, yet also, high life expectancy (3). The healthcare needs of the country have changed in recent decades due to an ageing and digitally more efficient population. 64.8% of the over-65 population live with comorbidity (4) and around 1 million people suffer with diabetes, asthma, COPD or cardiovascular disease (5).
There have been some positive changes in health service utilisation in recent years with the HSE workforce at its highest since 2006 (6) and a 24% reduction in the number of people waiting longer than Sláintecare targets for waiting lists (7). However, there is a lack of consistency across hospitals (8). Access to quality care across the country is needed, but not everyone is optimistic about the National Service Plans (NSP) 2024 budget and its ability to fulfil the needs of the people. Even the HSE Chief Executive Mr Bernard Gloster has publicly acknowledged that the HSE service plan ‘will include a built-in deficit because its 22.5bn budget allocation for 2024 […] is not sufficient to meet expected demand for service’ (9). Further stating that this amount will not be enough to overcome healthcare pressures, costs and return from the current deficit,
[…] it is nowhere near what is required to recognise the reality of the enormous increase in costs that have occurred within our sector.(10)
How can Ireland provide comprehensive and consistent access and inclusion to healthcare in 2024 when it faces budget insufficiency?
The Pursuit of Better Healthcare
As outlined in the NSP 2024, the Irish government has increased 2023’s budget by 4.6% for health and social care services. The top priorities for 2024 include delivering better quality and quantities of care throughout hospitals by increasing targets, providing additional beds, developing major trauma centres, and implementing the three-year Urgent and Emergency Care Plan (2024-2026). Waiting lists and times are included within the above, and will continue to be a top priority in the NSP. The multiannual Urgent and Emergency Care (UEC) Plan (2024-2026), will deliver immediate and long-term factors to improve the delivery of urgent and emergency care. This includes identifying and measuring the effectiveness of initiatives for hospital avoidance, emergency operations, in-hospital operations, and discharge operations. There will also be a focus on access to community care, including integrated care programmes for older people, chronic diseases, and home support. Promoting good mental health will address prevention and early intervention for child, adolescent, and adult services. Lastly, improved services within disability, with strategies to increase and retain the workforce in this sector, as well as improve access to support (e.g. respite, home support, etc.). Digital health is a named reciprocity of funding, which will further work towards the development of electronic health records, virtual wards, telemedicine, video consultations, wearables, and VR, to name but a few.
Digital Health in Ireland
Despite Ireland spending more of its national income on health than most European countries (11), without sufficient funding, Ireland will not fulfil the inclusive healthcare system that it aims for. However, it can improve, and it can work smarter to provide solutions that improve efficiencies and quality of care. This is echoed by Minister Donohoe’s statement for better, ‘productivity, better financial governance and consolidating funding capacity’ (12).
In the Digital Society and Economy Index (DESI) period: 2023, Ireland was ranked third for ‘at least basic digital skills’ and third for ‘above basic digital skills’ (13). Such positions should be leveraged within the country’s healthcare system. However, it is grossly underutilised, with Ireland ranking the lowest for digital health policies within the developed world (14).
Despite the rising growth of digital health in Ireland in recent years, funding for innovation remains the greatest barrier for those trying to make impact and change. While person centred care is often spoken about when discussing how digital health can impact many sectors across healthcare like diagnostics, prevention etc., funding pathways are deemed inaccessible. How can significant impact in healthcare be obtained when local and government authorities do not provide appropriate resource? (15)
The forthcoming Department of Health, Digital Health & Social Care Framework 2024 – 2030 is expected to forge the pathway to such positive change for consistency, innovation and utilisation of digital health. Ireland is in a unique position for positive change in digital health with a global reputation in life sciences and MedTech, and a ranking of number 2 in the 2022 World Index of Healthcare Innovation,
Ireland has a lot of ground to make up in digital health, but the tide is turning. When it does turn, it will bring significant change – and with that will come new challenges and opportunities. (16)
Design in Digital Health
Design ensures that health solutions are user-friendly and intuitive for patients, healthcare providers, and key stakeholders. Good design that emanates efficiency and usability helps to improve patient engagement and can influence perceptions of trust and credibility in the service or product. Moving forward, we cannot fail to appreciate the utility of design in future services and products, when pressures are high and funding is low. Now, as we move into an era whereby digital health is viewed as normality, design thinking principles will be the driver to creating impactful solutions for positive change. From intuitive interfaces to integration of data, from inclusivity to security and data privacy, by prioritising user experience, research and service designers can create solutions that both empower and improve outcomes. Design will be the driving force towards positive digital change in the health landscape.
With over 700 digital health companies in Ireland (including expanding sectors like MedTech and pharma) acknowledging the needs and potential of digital health solutions, digital design skills are becoming a recognised and attractive commodity.
‘The Irish digital health sector is uniquely focused on digital R&D as a key priority for upskilling.’ (17)
Investing in well-designed digital health services and solutions can achieve cost savings, improved patient outcomes, enhanced staff efficacy, increased patient satisfaction, and more. These factors contribute to the overall financial value of design in healthcare. While it can be challenging to quantify these benefits into a specific monetary figure due to the complex nature of the advantages, it is essential to break down the values that design in digital health provides, to segment appreciation where applicable.
- Well-designed digital health services can endorse operational efficiencies and produce cost savings.
Because design thinking places the user’s needs at the heart of the problem, delivering more appropriate solutions to that specific user within the wider context of the problem can impact flow in health. Whether that be the flow of staff, patients, patient families, information, medications, supplies, equipment, or output. This emerges from identifying inefficiencies in current flows, and leveraging what already works well while also implementing necessary change. The introduction of new or adjusted flows works because design includes the appropriate stakeholders throughout the process. With digital health, flows become even more efficient when design research and service design is included. With appropriate expertise and knowledge within the wider arena of healthcare, digital health, and technology, pivotal and positive change is possible – helping to save already pressurised healthcare systems from costs because of design-changeable/ preventative inefficiencies.
- Design interventions that prioritise patient comfort, safety, and accessibility can contribute to improved health outcomes
Designing easily navigable services creates a reassuring and positive experience within healthcare, which can help to encourage trust. Designers seek to understand the user’s needs and the user’s expectations of the service ensuring that patients are empowered on their health journey.
- Design can enhance staff efficacy by creating environments, tools, and processes that support and optimise the work of healthcare providers.
Creating better flows of information improves the accessibility of information, which in turn improves the efficiency of performing work tasks. Ensuring that the necessary means of communication for accessibility fosters appropriate channels for knowledge exchange. By incorporating design principles that prioritise the needs, preferences, and workflows of healthcare staff, organisations can create environments and tools that support staff efficacy, productivity, and job satisfaction. A well-designed intervention like ‘training, tools, organisational (re)design, and programmes’ can all assist to improve team efficacy in healthcare settings (18).
The Way Forward
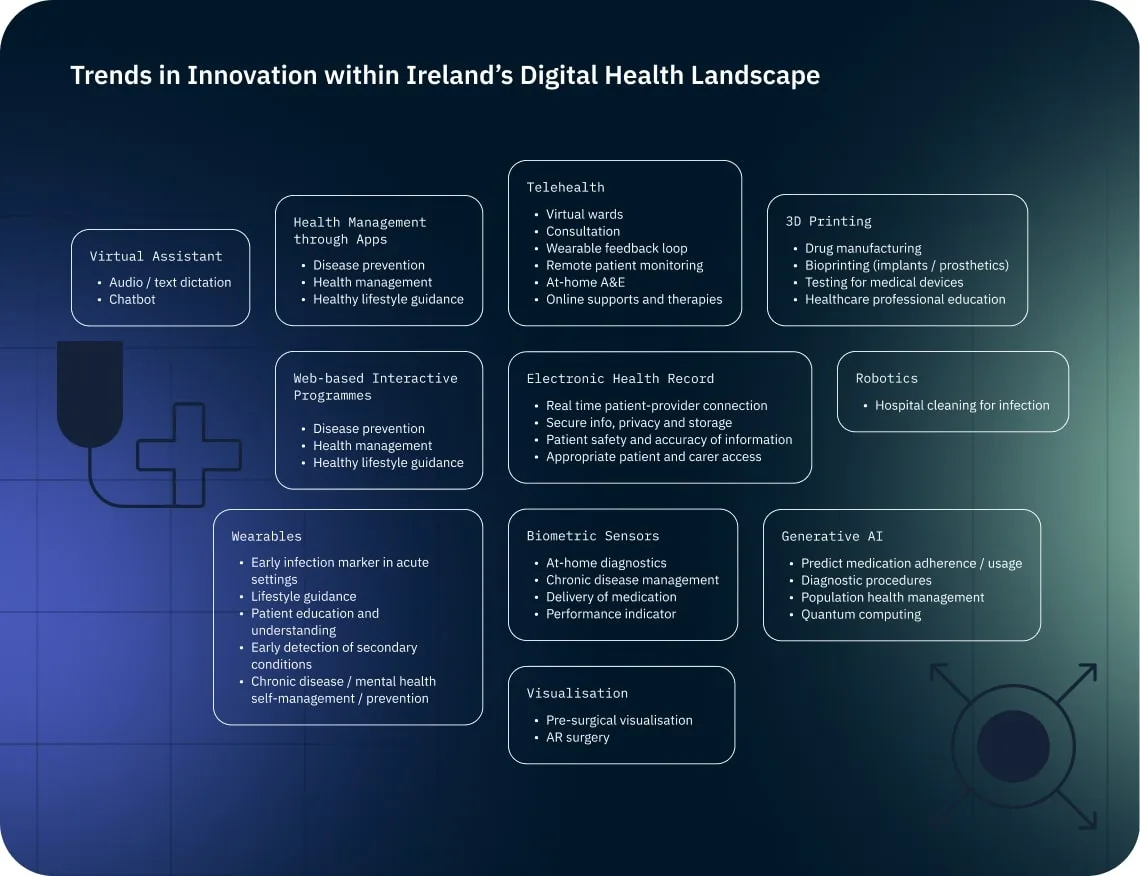
Optimistically, innovation is not in short supply within Ireland. Patient needs within threads of access and inclusion are being emphasised throughout Irish innovation – from wearables to 3D printing, personalised medicine to personal digital assistants. As trends go, digital health in Ireland 2024 is varied in focus across acute health, chronic health, and preventative health. The figure below provides trends of innovation observed within Ireland’s digital health landscape.
As Researchers and Service Designers, we’re inclined to feel motivated by the discrepancy between Ireland’s basic digital skills and its digital health policies, especially in light of the innovative trends observed. There is an opportunity for more user-centred input, ultimately creating and enhancing products and services in the digital health sector that are sustainable in Ireland’s complex health landscape. These can include:
- User Experience
- Efficiency and workflow improvement
- Data visualisation and insights
- Behavioural change and patient engagement
- Accessibility and inclusivity
- Empathy and human-centred design
Ireland has the potential to lead in digital health, globally, due to its continuing and burgeoning presence in the medtech and pharma sectors, as well as the blossoming presence of digital health start-ups. Together, through collaborative efforts and a shared commitment to user-centered design, we can drive positive change and contribute to the advancement of digital health services in Ireland. Let’s work towards a future where design helps improve digital health solutions and services to empower and enhance healthcare outcomes for all.
- 2_hse-digital-health-strategic-implementation-plan_fthompson_jward.pdf (ehealthireland.ie)
- Hse-digital-roadmap-web.pdf
- Health-Policy-in-Ireland-February-2016.pdf (drugsandalcohol.ie)
- The Irish longitudinal study on ageing, TILDA
- https://www.hse.ie/eng/about/who/cspd/icp/chronic-disease/#:~:text=Approximately%201%20million%20people%20in,cohort%20live%20with%20co%2Dmorbidity
- https://www.gov.ie/en/press-release/a6dc4-minister-for-health-highlights-increase-in-health-workforce/
- gov – Monthly waiting list figures – February 2024 (www.gov.ie)
- Hse-national-service-plan-2024.pdf
- Ministers furious at HSE chief executive Bernard Gloster over criticism of health budget | Irish Independent
- NHI, 2023, Health Budget 2024: Government misjudgement will intensify crisis in healthcare)
- chp_ir_english_0.pdf (europa.eu)
- gov – Statement by Minister Donohoe on Budget 2024 (www.gov.ie)
- DESI 2023 indicators – Digital Decade DESI visualisation tool (europa.eu)
- Ireland ranks worst for digital health policies in developed world, says report – The Irish Times
- Ireland, A Lack of Access to Preventative Care: A Call to Action for Policy Makers | ECHAlliance
- RCSI Online – Is there a lack of digital health readiness in Ireland? – Royal College of Surgeons in Ireland
- https://www.skillnetireland.ie/wp-content/uploads/2023/05/Where-Digital-Health-Thrives_Future-Skills-Needs-Analysis.pdf
- Interventions to improve team effectiveness within health care: a systematic review of the past decade – PubMed (nih.gov)
Discover more about Big Motive:
Big Motive is a digital design agency who focus on digital transformation, user experience and service design in healthcare. They help to shape how governments, healthcare providers, technologists and the public work together in achieving better health and health-related outcomes.