As medical advances continue to extend human lifespans (adding 15 years in the western world since only 1980!), achieving healthy aging has become a top priority for individuals and societies alike. Living not just longer but better—with greater vitality, mobility, and independence—is the goal. However, aging is a complex, multi-factorial process influenced not only by genetics and lifestyle choices but also social and environmental conditions. To truly optimize health-span, we must take a holistic, population-level approach that considers all the factors impacting human well-being.
Fortunately, emerging technologies now allow us to gather and analyze rich health data from entire populations in unprecedented ways. By leveraging these tools, innovative programs are gaining deeper insights into aging and identifying strategies for thriving at every stage of life. This “population health” model holds great promise for supporting longer, healthier lives for all.
A Population Health Perspective on Aging
Traditionally, healthcare has focused on treating illness on an individual basis. But aging results from the combined effects of innumerable influences, from genetics and behaviors to social connections and community resources. This suggests that we can get better results by taking a broad-based population health approach, which means examining how these diverse factors interact across entire groups of people over time. For example, electronic health records provide longitudinal data on diagnoses, treatments, outcomes, and more for entire patient populations. Wearable devices and mobile apps continuously monitor behaviors, activities, sleep patterns, and other lifestyle metrics in real-world settings. Community surveys gather information on social determinants of health like income, education, housing, and access to services.
By integrating these diverse data sources, researchers gain a multidimensional view of how health and well-being evolve within specific populations as they age. This reveals which combinations of factors most powerfully drive outcomes like disease, disability, and quality of life. It also pinpoints opportunities for targeted interventions addressing root causes, rather than just symptoms, of ill health.
Leveraging Technology and Innovation
Technology is further fueling population health innovation through new models of care delivery. For instance, remote patient monitoring uses devices, apps, and telehealth to collect clinical measurements outside traditional healthcare settings. This allows ongoing surveillance of health indicators such as blood pressure, weight, and glucose in patients’ real-world environments. AI and machine learning algorithms then analyze these massive, real-time data streams. They can detect subtle changes signaling worsening conditions early, when interventions are most effective. The algorithms also reveal patterns and predict future risks, guiding more proactive, preventive care. Telehealth further ensures all populations, regardless of location or mobility, can access expertise when needs arise.
Wearables and sensors are also empowering individuals to play a more active role in their own health maintenance. By providing continuous feedback, these tools help people modify behaviors and catch issues promptly. Communities and support networks then reinforce these efforts through shared data, mutual accountability, and collaborative goal setting. Over time, population-wide behavior change becomes self-sustaining through grassroots social support structures.
A Holistic, Multidisciplinary Approach
Of course, optimizing health and wellness requires attention to all aspects of life, not just medical factors. Population health innovators are thus adopting comprehensive, multidisciplinary models. For example, some programs pair clinical interventions with social programs addressing needs like nutrition, housing, employment, and loneliness—the so-called social determinants of health. Public and community health experts can now more effectively design “age-friendly” environments, making communities safer, more accessible, and socially engaged. This can include recommendations around better health and ways to thrive, such as more walkable streets, accessible transportation, and opportunities for social participation, all of which influence well-being.
Collectively, these holistic, technology-enabled approaches consider the full spectrum of factors impacting population health and longevity. By addressing physical, behavioral, social, and environmental determinants together, technology-enabled approaches stand to optimize health and quality of life for older adults far beyond what any single intervention could achieve. Ongoing evaluation ensures continuous improvement, with the goal of sustaining health and independence for as many years as possible.
The Future of Healthy Aging
As population health innovation advances, its potential to transform aging experiences is immense. With ongoing data collection and research, programs will grow ever more tailored and effective at addressing the unique needs of specific populations over time. Individuals will gain powerful self-management tools and support systems for lifelong wellness. Communities will become increasingly age-friendly through data-driven improvements.
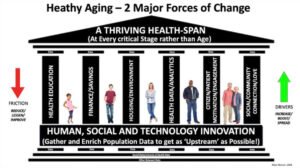
One model for thinking about how we might strategize around healthy aging is shown in the diagram below. This suggests a simple analogy to erecting a stable edifice upon which we can build on solid foundation—in this case, population health data gathered with individual human, social, technological, and other innovation needs in mind. The diagram also suggests that we can think carefully about many contextual factors that impact our short, medium, and long-term health, including education, finance or capacity to pay, housing, and our physical environment, the quality of the data we collect and analyze, citizen and community engagement, and finally how people socialize and connect. A thriving HealthSpan, the final goal—or the roof as it is shown here—is the ultimate outcome we achieve, not just in older age but at every stage of life. Finally (and at the far left and far right of the chart below), we should be careful to manage the two major forces of change: The friction forces that can hold change back or slow it down, and the boosting forces or drivers that help change happen more readily or even quickly.
More people than ever before want to remain active, engaged, and independent well into their 70s, 80s, and beyond. With continued progress, humanity may even approach the theoretical limit of the human lifespan while disease and disability remain at bay. It’s an exciting future if we strategize for it well today and make the investments to bring the changes into being.
To this end, I will be leading a session on Healthy Aging at the HLTH Conference in Las Vegas on Sunday, 20th October, as part of the ECHAlliance Partner Program. This exclusive event will focus on Women’s Health, Healthy Aging, and the transformative role of Data & Digital innovation. The programme will run from 13:00 to 16:00, featuring expert speakers and thought leaders discussing key innovations in healthcare.
From 20th to 23rd October, you can also visit the Global Health Connector Village to explore the latest in digital health, with sessions on the Village Stage throughout the event.
If you’re still interested in showcasing your innovations, you’re still on time to become an exhibitor at the Global Health Connector Village.
This article was written by Jon Warner, Executive Chair of Citizen Health Strategies (CHS) and US Ambassador for the ECHAlliance – The Global Health Connector.

