
If you tell people something is going to hurt, it is going to hurt and every adult will recognise this from their own experience. We also need to remember that, unfortunately, some people also have a phobia of needles. So what about children who, for example, have to have a blood test, have skin flakes removed or have a skin biopsy?
Focus language: a tool for caregivers and parents
If you tell people something is going to hurt, it is going to hurt and every adult will recognise this from their own experience. We also need to remember that, unfortunately, some people also have a phobia of needles. So what about children who, for example, have to have a blood test, have skin flakes removed or have a skin biopsy? How can we prevent a child from suffering a trauma? After all, there is always a first time for a child in its journey to adulthood. “A child is not a small adult,” says Elodie Mendels, who is a paediatric dermatologist at Erasmus MC in Rotterdam.
Mendels first outlines the context. “Fear and pain can traumatise children. Therefore, avoiding pain and fear in children should be as important a goal as the medical procedure itself.”
How can we make the care of children trauma-free?
“What it’s all about is creating trust. This is because patients who have confidence in their treatment and practitioner experience less pain and stress, heal faster, have fewer traumatic memories and also retain confidence in care.”
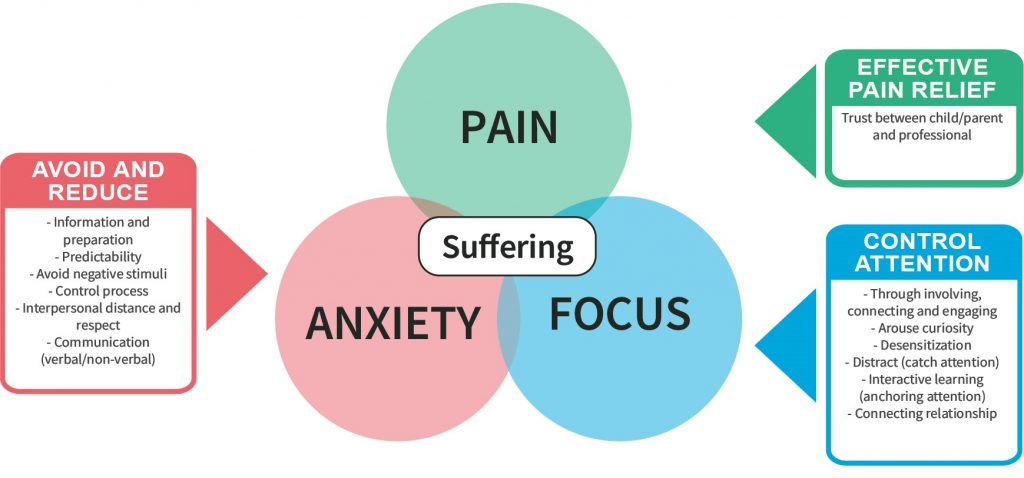
“Pain, anxiety and stress during medical procedures are preventable in most cases. There are many different techniques available to achieve this, but you have to use them in the right way, at the right time and in the right situation. These techniques act on three issues: pain (for example, by relieving pain with medication), fear (reducing fear, for example, by proper information and preparation, managing expectations and organising predictability so avoiding unexpected events), and focus (including shifting focus so that less fear and pain occur, for example, by using a relaxation exercise, game or digital distraction tools). What is needed is a multi-faceted approach that aims to achieve short-term comfort during the treatment, success of an intervention, and long-term preservation of the child’s and parent’s trust in the care provider.
Parents are also very important in creating trust and can contribute something substantial to the trauma-free care of children, together with the doctors. Mendels zooms in on ‘focus language’ as a tool for parents and caregivers: “Focus language is a very practical technique and parents can apply it immediately.”
Focus on language
“Everyone does their utmost to communicate well,” says Mendels, “I am convinced of that. However, not every approach leads to the desired result of reassurance. Well-intentioned advice can also have the wrong effect. The result is that, instead of reducing or eliminating a child’s fear, doctors and parents reinforce it.”
Name a few approaches that should be avoided?
“The use of coercion – physical and psychological – to suppress a child’s resistance to an operation is still often used and of course this is never good for a child. Examples of other approaches that can lead to distress are for example, giving a child incorrect or misleading information. For example, when using a needle with a child, comments such as …
“It will only take 10 seconds.”
“3, 2, 1, here comes the prick!”
“We’re almost done, shall we count down from 10 together?”
“Sorry, this is really mean!”
These are all classic examples that can create anxiety in a child, incidentally and despite the good intentions.”
How can – and should – it be done differently?
“We need to shift the focus. How? By using different language and adopting a different attitude. In professional circles, this is called ‘focus language’. It is an approach that has long been used in relaxation and distraction techniques. The emphasis is on positive reassurance and in this way, through the choice of words, one can shift the patient’s attention. You take the negative charge and words out of a conversation, as it were. The fact that choice of words can have a positive effect on the perception of fear and pain is not rocket science. These positive effects have now been extensively confirmed in the scientific literature.”
Mendels cites some examples. “By using different language, for example, there are 40% fewer interruptions of MRI examinations, which many people with mild claustrophobia are afraid of. In addition, various treatments go faster because patients are less anxious and tense, and patients experience more confidence in the care. “It seems easy at first glance but it takes some practice. It is worth the effort because there is a world to be won.”
Classic mirroring
“Another effective tool is the so-called mirroring of the patient as non-verbal communication. If the healthcare provider adopts the patient’s body posture, the patient unconsciously feels more understood. Mirroring shows that people connect more quickly and feel more understood and more comfortable. This can help in certain situations. Even if it means that I have to sit next to the child for a while with my legs dangling over the edge of the examination couch.”
Her final chord: “Skin procedures without fear and pain are really possible and the great thing is: we can all do it because it’s in us as human beings: understanding, respect, empathy and trust.”
“What it’s all about is creating trust.”
Positive focus language: do’s and don’ts
Preparation
- Introduce and use language at the child’s developmental level.
- Is the child prepared? If yes: Ask the child to explain to you what he knows or has experienced before. If not: Ask if there is a need for preparation and what words parents might give to actions and materials.
- If the child is prepared: Ask if the child needs monitoring or ‘blunting’.
Monitoring: the child wants to know what is happening. Involve the child in the procedure. Explain what is happening.
Blunting: The child wants to be distracted during the action. Ask in what way and see how this can be given shape.
| Do this | Don’t do this |
|---|---|
| For example: ‘We are about to remove a piece of skin. Do you like it when I tell you how we are going to do it?’ If so: ‘First, you will be given a plaster with ointment to numb the skin {watch out for Emla; 60-90 min; Rapidan; 30-45 min}. [2] on the spot where we are going to remove the piece of skin. Then you go and wait in the waiting room with (… mummy – daddy etc.). In (… half an hour) I will pick you up. Then I will tell you what we are going to do next. OR: ‘Then we will put extra anaesthetic into the skin. And then we will take away the piece of skin. You will see how well we can do this together’ (create trust).’ | For example: ‘We are about to take a skin biopsy with this apple corer. It is very small. See? First you get a little prick. It will feel a little burning/painful. Then we count down together. Then the skin is numb and we take the biopsy. Sometimes it still hurts a little, but it’s actually not that bad.’ |
| ‘Do you want to sit on mummy’s lap when we (remove the skin/ give the medicine/ remove the dander/ …) or do you want to lie on the couch?’ {Do not give the child the choice of whether we are going to do it, but how it is going to happen. The child will then experience a sense of direction and trust}. | Forcing the child to sit on the examination bench: ‘Come on, shall we do it now?’ Common response: ‘No, I don’t want to!’ ‘It’s over in a flash, so come on.’ ‘I won’t hurt you/It will be a little uncomfortable, but it will be over soon/Come on, there are more children waiting and they are all waiting for you/I don’t have all day/I promised I wouldn’t hurt you/you are a very tough boy/girl, so let’s do it now.’ |
| ‘You may like to sit or lie down.’ (admitting language) | ‘Sit down or lie down.’ (directing language) |
| ‘Do you want to watch what we are about to do or do you prefer to do something while we are busy giving the medicine/ ….?’ {If the child is more comfortable doing something (blunting), you could, for example, let them choose something from a box of ‘distraction objects’, such as a search book, a magic wand, bubble blowing, digital distraction techniques etc. Parents often have good ideas of their own for distraction} | ‘Are you afraid of needles? Then I wouldn’t look!’ ‘Don’t worry about it!’ ‘It’s not that bad!’ ‘You just need to relax!’ |
During operation
| Do this | Don’t do this |
|---|---|
| ‘Because you are so good at lying still, I can do … good.’ | ‘It only takes a moment.’ |
| ‘It’s good that you’re lying still, this way the examination can be completed more quickly.’ | ‘You mustn’t move, otherwise …’ |
| ‘I wonder how well you can lie still.’ | ‘Try to lie still.’ |
| Link the puncture to the exhalation (e.g. when blowing bubbles). | ‘Asking permission (‘Can I give you the shot?’). Warning (‘Here you go!’) and counting leads to more fear and pain. |
| ‘I’m curious to see how quickly and/or well the medication/anesthetic will work on you. You’ll notice how quickly your arm feels good again.’ | ‘The needle prick only hurts for a moment.’ |
| ‘I’m going to give you the anesthetic now and then …’ | ‘The injection is not nice, but then I can take the skin piece without pain.’ (but it destroys something and that sticks).’ |
| ‘and because you now … (something positive) you will notice that …’ | ‘Do not worry so much!’ |
| ‘And while you breathe in and out slowly, you will notice that you become calmer and … (examination/treatment) will go easier and faster.’ | ‘Calm down, you’ll be fine!’ |
| ‘I wonder how well this works for you.’ | ‘We hope….’ (so it doesn’t have to work).’ |
| ‘You’ll be surprised how easy it is if … for example you take a good look at the magic bird on your finger and let it fly / you tell me what you can see in your video.’ | ‘I wonder if you feel anything about it.’ ‘It’s ready soon!’ |
Reframe pain/other complaints
| Do this | Don’t do this |
|---|---|
| ‘Je zult verbaasd zijn hoe snel je arm weer goed voelt na …’ ‘Je zult benieuwd zijn hoe snel je je beter voelt.’ | ‘The prick only hurts for a moment.’ |
| ‘Everyone experiences (…) differently, I am curious what you think of it/how you experience it.’ | ‘Many people get very dizzy from this/most people find it a painful puncture.’ ‘Yes, I’m sorry, this pain is really bad.’ |
| If you want to name the sensation: ‘Tickling, scraping, tingling’. | ‘Burning, stinging, aching, hurting, bad, nasty, horrible.’ |
| ‘If there is anything, please let me know. Then I can help you.’ | ‘You can get sick from this. Here is a spit bucket for you.’ |
Evaluation
Always evaluate, because this constructs a proper memory and increases confidence in future medical acts.
| Do this | Don’t do this |
|---|---|
| ‘I wonder if today or tomorrow or very soon …’ (and then mention a positive change) | ‘I hope you will feel better tomorrow than you do now.’ |
| ‘It went well.’ | ‘Yes, sorry, that was painful, but you did a good job.’ |
| ‘And how did you think it went?’ | ‘Until next time, go home.’ |
Source: Heel de Huid (NVDV, Utrecht, the Netherlands). December 2021.
Photography: Roos Koole
Discover more about CMTC-OVM:
CMTC-OVM is the worldwide non-profit patient organization that aims to improve the quality of life of people suffering from vascular abnormalities (blood vessel abnormalities), such as CMTC (‘Van Lohuizen syndrome’), and stimulate scientific research into these disorders.
Our commitment is to support the welfare, foster well being of our patients and support the scientific research of vascular malformations such as CMTC.
The patients in our organisation have the unique opportunity to get the best research of the causes, diagnosis and the best treatment of issues related.
We not only support patients but also their families both medically as well as psychologically.
